Telehealth systems can be models of future healthcare

Telehealth, or telemedicine, began as a means to treat patients in rural areas, those who were situated too far away from healthcare facilities or professionals. It has since become a tool for convenience, as patients today turn to telehealth for immediate, virtual consultation and care.
Although the recent COVID-19 pandemic sped up the adoption of telehealth since physical consultations were restricted and this helped reduce the risk of infection, there are, however, marked challenges and limitations to today’s telehealth systems that can be addressed to prove more efficient in the future.
Consulting firm Roland Berger’s latest study, “Telehealth 2.0: Expanding the reach of healthcare in Asia Pacific” uses Orthopaedics to explore telehealth systems’ current challenges and opportunities; it has denoted three such challenges:
- Telehealth is not a one size fits all solution – the telehealth models built for acute episodic care may not be effective for patients that require constant reviews and chronic care, such as ageing societies;
- Teleconsultations will not be able to deliver the best results without physical examination(s) such as to assess several motor tests more accurately. A lack of centralised access to imaging repositories also delays accessibility to patients’ records;
- Telehealth systems in Asia Pacific lack infrastructure development – various markets are underserved and suffering from a shortage of diagnostic facilities such as the DEXA scan machines, which help detect bone disorders. These same markets face risks including the potential loss of healthcare data or incorrect data input.
The study also identified six telehealth business model platforms in Southeast Asia, namely – health information, primary care access, primary care+ access, organisation-to-organisation connector, health ecosystem orchestrator and asset-light healthcare providers. These will allow the swift advance of telehealth from a service to an ecosystem enabler.
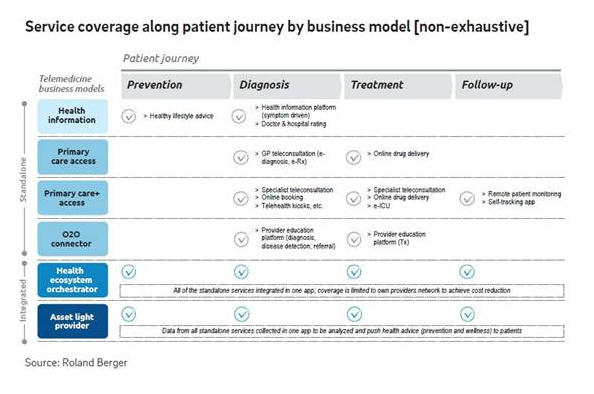
For example, the primary care+ access model, a platform for amplified care, provides referrals/assistance with patient’s access to tertiary care including diagnostic centers, specialty care providers, hospitals, rehabilitation centres and pharmacies, in addition to GP services. However, in most cases, the platform does not have full integration with the rest of the healthcare stakeholders.
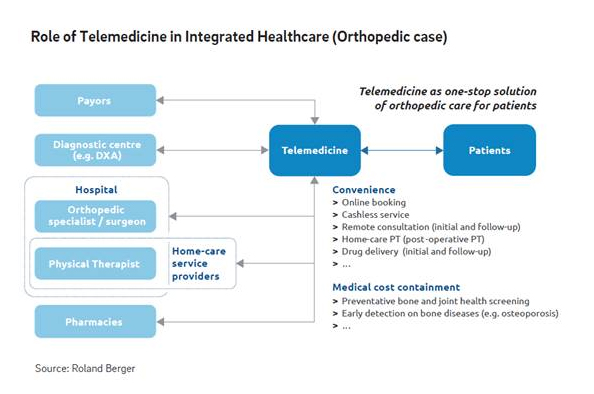
An integrated option is the health ecosystem orchestrator, a telehealth model which coordinates more complex interactions and transactions between patients, providers, payors and other healthcare stakeholders. The orchestrator usually enables care by going beyond the traditional channels and partners with adjacent players who have stakes in a healthier population like banks, telecoms and retail. Through the orchestrator model, services such as insurance claims, follow-up consultations or drug deliveries are all easily accessible and arranged via one platform. While the challenges of standalone models can be mitigated, this model also ensures affordable healthcare for the community by keeping patients within the same healthcare network.
Stakeholders – including tech-startups, medical tech and pharmaceutical companies – are also required to extend support towards the digital transformation of the healthcare system, especially in Asia Pacific: policymakers and regulators should develop supporting policies to enable telemedicine and define standards and protocols to help reduce inefficiencies, for equitable healthcare; healthcare providers should begin instituting synchronous models and invest in infrastructure for seamless online to offline integration; payors with incentive-linked programs can significantly influence patient’s behaviour on choosing preventative care and wellness, while health insurers can digitally steer their customers toward a network of preferred partners.
Read: Managing the strain on healthcare through digitalisation





